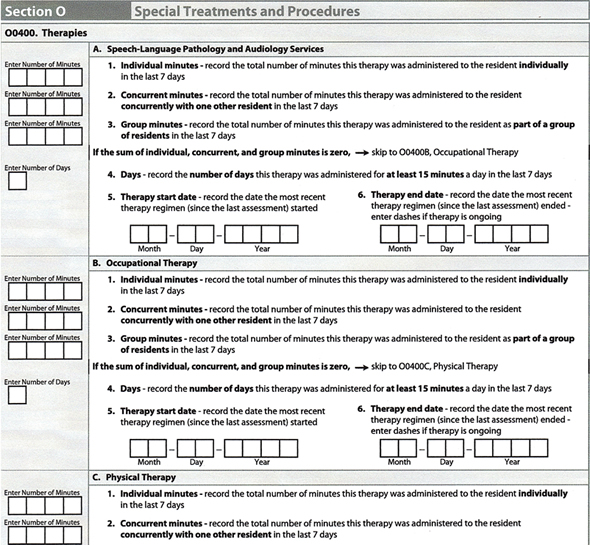
Let’s start by talking about how the therapy days and minutes will be reported on MDS 3.0.
Each therapy discipline will continue to report the number of days and minutes therapy was provided in the last 7 calendar days. However, they will now be required to separate the type of therapy delivered into the following modes of therapy:
Individual
Concurrent
Group
 Individual minutes are minutes provided to a resident one-on-one.
Individual minutes are minutes provided to a resident one-on-one.
Concurrent minutes are described as the treatment of 2 residents at the same time, when the residents are not performing the same or similar activities, regardless of payer source, both of whom must be in line-of-sight of the treating therapist or assistant. For Part B, residents may not be treated concurrently; minutes provided with 2 or more residents would be recorded as group minutes. CMS is very clear that there is a limit of 2 residents for concurrent therapy. If the therapist is treating 3 residents at the same time, not performing the same or similar activities, no minutes can be coded on the MDS for any of the residents during that treatment time.
Group therapy minutes are described for Part A as the treatment of 2 to 4 residents, regardless of payer source, who are performing similar activities, and are supervised by a therapist or an assistant who is not supervising any other individuals. For Medicare Part B, treatment of two patients (or more) at the same time regardless of payer source is documented as group treatment.
The days that therapy was provided continue to be as important to the RUGS calculation as the number of minutes. In order to count a day of therapy, at least 15 minutes of skilled therapy must have been provided during the calendar day. 15 minutes or more of concurrent therapy would qualify for a therapy day even though the grouper will divide the total minutes in half. If the total number of individual, concurrent and group minutes equal zero, skip this item and leave blank.
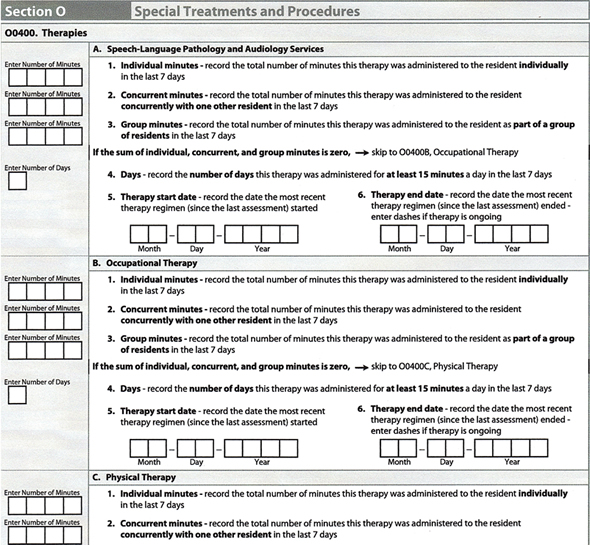
The therapy start date is the date the initial therapy evaluation is conducted regardless if treatment was rendered.
The therapy end date is the last date the resident received skilled therapy treatment. Enter dashes if therapy is ongoing.
One of the biggest changes in MDS 3.0 is the elimination of Section T—estimated days and minutes of therapy projected to be provided during the resident’s first 15 days from admission.
Selecting What Type of Assessment
If a therapy RUG can be obtained using the standard 5-day PPS assessment, that is usually the best assessment choice for payment. When the resident has been in the facility less than 8 days and has not received enough days or minutes of therapy to qualify for a Rehab RUG on the 5-day PPS assessment, a short stay assessment may be possible. There are 8 requirements that must be met before a short stay MDS can be completed.
The 8 requirements are:
- The assessment must be a Start of Therapy OMRA (SOT). This assessment may be completed alone or combined with any OBRA assessment or combined with a PPS 5-day assessment. The SOT OMRA may not be combined with a PPS 14-day, 30-day, 60-day, or 90-day assessment. The SOT OMRA should also be combined with a discharge assessment when the resident discharges from the facility. However, if the resident expires in the facility or is transferred to another payer source while in the facility, do not combine the SOT OMRA with the discharge assessment.
- A PPS 5-day or readmission/return assessment has been completed. The PPS 5-day or readmission/return assessment may be completed alone or combined with the Start of Therapy OMRA.
- The ARD of the SOT OMRA must be on or before the 8th day of the Part A Medicare stay. The ARD minus the start of Medicare stay date must be 7 days or less.
- The ARD of the SOT OMRA must be the last day of the Medicare Part A stay. The SOT OMRA ARD must be the end of the Medicare stay date. The end of the Medicare stay date is the date Part A ended.
- The ARD of the SOT OMRA may not be more than 3 days after the start of therapy date. This is an exception to the rules for selecting the ARD for a SOT OMRA, as it is not possible for the ARD for the Short Stay Assessment to be 5-7 days after the SOT since therapy must have been able to be provided only 1-4 days.
- Rehabilitation therapy (speech-language pathology, occupational therapy or physical therapy) started during the last 4 days of the Medicare Part A covered stay (including weekends). The end of Medicare stay date minus the earliest start date for the three therapy disciplines must be 3 days or less.
- At least one therapy discipline continued through the last day of the Medicare Part A stay. At least one of the therapy disciplines must have a dash-filled end of therapy date, indicating ongoing therapy or an end of therapy date equal to the end of covered Medicare stay date. Therapy is considered to be ongoing when:Resident was discharged and therapy was planned to continue had the resident remained in the facility
Resident’s SNF benefit exhausted and therapy continued to be provided
Resident’s payer source changed and therapy continued to be provided
- The RUG group assigned to the Start of Therapy OMRA must be Rehabilitation Plus Extensive Services or a Rehabilitation group. If the RUG group assigned is not a Rehabilitation Plus Extensive Services or a Rehabilitation group, the assessment will be rejected.
If all eight of these conditions are met, then MDS Item Z0100C (Medicare Short Stay Assessment indicator) is coded “Yes.” The assignment of the RUG-IV rehabilitation therapy classification is calculated based on average daily minutes actually provided:
15-29 = Rehab Low
30-64 = Rehab Medium
65-99 = Rehab High
100-143 = Rehab Very High
144 or greater = Rehab Ultra High
Interviews
The addition of the resident interviews, which requires completion of the interviews on or before the ARD, impacts the ability to move the ARDs in the PPS windows. The therapy director and MDS coordinator will need to continue to work closely and maintain good communication with the entire IDT team.
The addition of the discharge assessment adds another dimension to the MDS 3.0 process. The discharge assessment includes therapy days and minutes and can affect payment when combined with other PPS assessments. Be sure to keep your team informed of changes in discharge dates, therapy start dates and therapy end dates.



 Carlos Jaimes in Rehab at Whittier Hills Healthcare Center, always goes above and beyond for the residents. One of the patients he was treating in therapy had spilled something on a jacket that she wanted to wear that day. The jacket needed to be hand washed, so Carlos took it on his lunch break back to Laundry and hand washed the jacket for this resident. Carlos is always ready to help out wherever and whenever he is needed—whether it is part of his job description or not.
Carlos Jaimes in Rehab at Whittier Hills Healthcare Center, always goes above and beyond for the residents. One of the patients he was treating in therapy had spilled something on a jacket that she wanted to wear that day. The jacket needed to be hand washed, so Carlos took it on his lunch break back to Laundry and hand washed the jacket for this resident. Carlos is always ready to help out wherever and whenever he is needed—whether it is part of his job description or not.



 Individual minutes are minutes provided to a resident one-on-one.
Individual minutes are minutes provided to a resident one-on-one.