Understanding, Preventing and Managing Challenging Behaviors – A Cognitive Link
By Pat Jakubiec, Clinical Resource
Challenging behaviors are one of the most stressful aspects of care giving. They result in caregiver stress, excess disability and increased care costs. Recent research suggests that pharmologic approaches are not always effective and they can cause potentially harmful secondary side effects, including an increased risk for falls. Research shows promise for engagement in meaningful activity tailored to an individual’s ability can reduce depressive and agitated behaviors as well as reduce caregiver stress.
Behavior is a way individuals express a need or desire. It can result from an emotion, and sometimes the behavior remains the focus not the emotion (Pollard, 2005). Individuals with cognitive disabilities can be misunderstood and sometimes blamed for their behavior. The reason is usually related to underlying neuro-biological causes that include global cognitive abilities, speed of brain function and personality traits.
Every change in a person’s environment will require the individual to cope and adapt, using extra effort and energy. Many people with cognitive impairment are not able to learn to adapt to new routines, procedures and physical changes in the environment. The individual biologically has difficulty noticing and processing information, therefore they cannot use the information to influence behavior. Functional performance beyond an individual’s ability cannot be expected especially in novel situations. When this occurs, performance failures can be anticipated.
Some researchers describe the anterior cingulate cortex of the brain as a key area between thought emotion and the body’s response to what the brain is feeling. An individual’s responses represent value judgments within a social context. The individual with cognitive disability often times has difficulty understanding the full scope of the social environment and difficult behaviors can represent this challenge. When the brain declines in its ability to work as a global unit, agitation can be viewed as a loss of control over behavior and the ability to process the environment.
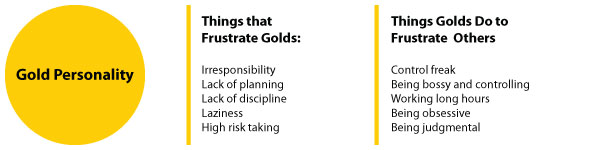
There is a fine balance between doing too much for the individual that may lead to depression, excess disability and a decreased sense of self. Doing too little can result in agitation, problematic behavior and an increased risk for accidents. It is important to assess an individual’s abilities and personal factors in the context of holistic assessment. The degree or level of behavioral reaction can be attributed to an individual’s personality traits and how they have handled life situations.
In 1995 Cohen-Mansfield described behavioral symptoms into 4 groupings:
- Physical aggressive behaviors
- Verbally aggressive behaviors
- Non-aggressive physical behaviors
- Non-aggressive verbal behavior
A careful medical assessment needs to be included. Certain conditions and illnesses, unmanaged pain, and medication changes all need to be considered.
Environmental assessment and management become critical. Changes in the physical environment can cause challenges as the person may have difficulty processing the physical space. Consistent nurse aide assignments with ongoing team education provide a supportive human environment. Integrating lifelong habits and routines promotes cognitive strengths and a sense of self. An integrated environment promotes overall feelings of well-being and security.
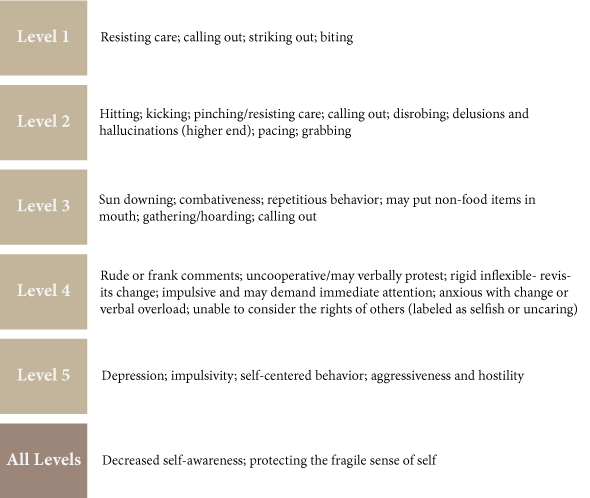
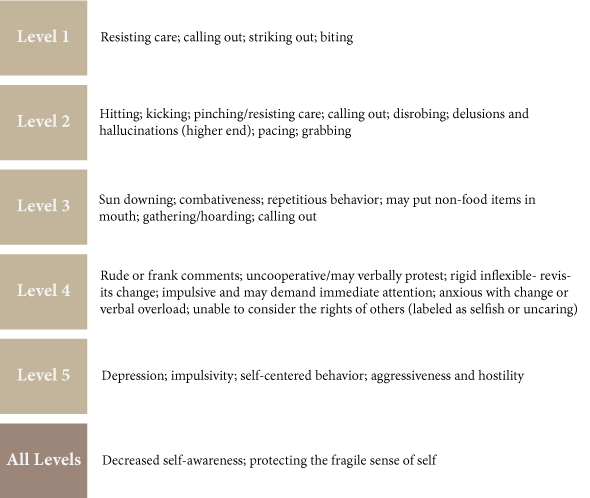
Use of the cognitive disabilities model allows healthcare clinicians to understand different levels of global brain activity. The six levels (ACL scale) describe distinct patterns of behavior that can be anticipated. These behaviors can be measured and managed by skilled clinicians, offering a cognitive systematic approach to management and intervention. Strategies can be developed integrating personal factors that can be employed by everyone. This provides a pro-active approach to care and may prevent some challenging behaviors before they occur.
Behavior Patterns Observed in the ACL Scale
Bathing Challenges/Process
Resisting care, especially during bathing is a common challenge that causes distress for both the individual and the caregiver. Interventions are meant to be used as a guideline and are meant to be modified by the treating therapist in the context of a comprehensive holistic assessment.
Reasons for referral
- Recent decline in function and or participation
- Resisting care- verbal or physical aggression
- Refusing or withdrawal
- Individuals requiring more than one nurse aide to complete bathing /showering
- Issues of safety associated with bathing and showering
Evaluation
- Complete a comprehensive holistic assessment
- Establish a functional cognitive level through the use of at least 2 standardized tools and observe a stable pattern of behavior
- Have the family complete an Advance Lifestyle Directive “Life Story gathering instrument.” Gather as much data related to the person’s lifelong bathing/ showering habits to include time of day, types of products used, frequency, preferences etc.
- Observe the person and caregiver in the actual task environment
- Identify problem behaviors observed and any identifiable patterns of difficult behaviors. (frequency, duration intensity)
Intervention
Clinical analysis of behaviors. Many behaviors can be an expression of an unmet need. This may include:
- Feeling cold; fear; pain
- Embarrassment/vulnerability
- Loss of control
- Not able to process the environment, or understand what is happening
- Fatigue
- Unable to understand what the caregiver is communicating
Compare cognitive level with actual task participation. If excess disability is present determine why and what therapy interventions can be done to improve participation. When excess disability is cognitively related sometimes the caregiver approach can be modified to improve outcomes. This is often witnessed when people are functioning in Allen Cognitive Level (ACL) 3.
Develop a plan to reduce problematic behaviors, maximize patient participation and profile effective communication. Things to include in the plan are:
- Time of day (avoid bathing when fatigue is present, life habit)
- Use of familiar items
- Integration of preferences and lifelong habits/ mode of bathing
- Communication strategies
- Physical environment considerations (room temperature, water temperature, unfamiliar location or change, privacy, noise level, past familiar environment, comfort)
- Pain management strategies
- Strategies for participation
- Safety
Provide treatment sessions to implement and modify strategies and to train the caregiver in the actual task environment.
Document the plan and caregiver training.
Develop a functional maintenance program.
Follow-up with caregivers during and after the procedures have been completed, and note what has been successfully achieved.
Conclusion
This information was adapted from the VCIM Clinical Guide for Understanding, Managing and Preventing Challenging Behaviors. Some of the facilities using this approach have shown a reduction in falls, combative behaviors, reduced use of restraints and reduced use of psychotropic medications. For more information, contact Pat Jakubiec at pjakubiec@ensigngroup.net. Onsite clinical development and training sessions and skype case study consultation are available. Staff development and training is tailored to individual program needs.



 Get patients to the next Level of Care in a shortened amount of time, with quality outcomes.
Get patients to the next Level of Care in a shortened amount of time, with quality outcomes. Manage clinical needs and financial implications according to contracted levels.
Manage clinical needs and financial implications according to contracted levels. Goals should be written according to specific prior level of function.
Goals should be written according to specific prior level of function. Begin working with patient/ family from day 1 to determine a reasonable and achievable discharge plan.
Begin working with patient/ family from day 1 to determine a reasonable and achievable discharge plan. Meet weekly with the clinical team to discuss progress/ barriers to goals.
Meet weekly with the clinical team to discuss progress/ barriers to goals.