For the first time ever, Willow Bend Nursing and Rehabilitation Center has won the most elite 2014 Ensign flag award! We are so honored and blessed to work here.
For the first time ever, Willow Bend Nursing and Rehabilitation Center has won the most elite 2014 Ensign flag award! We are so honored and blessed to work here.
Willow Bend Nursing and Rehabilitation is a 162-bed skilled nursing facility in the heart of Mesquite, Texas. Willow Bend has been voted the best rehab in Mesquite for two years in a row. We pride ourselves on improving year after year in almost every significant measurement.
We have overcome many major hurdles, such as: 1) A brand-new skilled nursing facility opened up in between our number one referring hospital and us, and 2) We have taken on rising costs, such as hiring an additional case manager, increasing our MDS nurses from two to three and strengthening the number of employees involved in the admissions process. Despite these challenges, we have been able to increase our EBITDAR Margin. We have implemented many new programs this year to increase our employee and resident satisfaction, and we truly continue to grow as a staff. We are always striving to meet the needs of our community to remain the best SNF in our community.
Our leadership team is phenomenal! We have all directly impacted the course and future of our building and its programs:
Allen Mall, Director of Nursing: Allen became Willow Bend’s DON in 2013 and has led our facility to extraordinary clinical results. With Allen’s excellent leadership, we were able to improve our staff’s skills and education to enable us to complete our January 2015 Survey with only one low-level nursing tag. Allen has channeled his passion for nursing and the Ensign way to drive our team to strive for the excellence of an Ensign flag facility.
Allen has challenged every employee to be the very best they could be. Under his leadership, Willow Bend has been able to create a hard-working and dedicated team that truly cares for each other and our residents. Allen has helped to create a desire in employees that no matter how difficult the journey may be, we should strive to not only be one of the best within Ensign, but also the best in our community. Allen’s passion is infectious, and Willow Bend is truly blessed to have him as our DON. We are sure in the years to come that he will help our facility continually shine as a proud part of the Ensign Group.
Linda Herndon, Director of Marketing: Willow Bend is blessed to have Linda Herndon as the Director of Marketing since 2008. Willow Bend has been in the Mesquite area for over 50 years, and it did not have a good reputation. This is where Linda’s difficult job of transforming Willow Bend began. The community was not receptive because of Willow Bend’s past reputation, so Linda started developing relationships with physicians in the community. It took time to gain their confidence and give us a chance to show the level of care of which Willow Bend is capable.
The reputation began to develop and vastly improved as a result of Linda’s relationships and the great team that worked together to prove we provide quality, loving care. We all shared our peaks and valleys together, which proved to our residents, families and referral sources that the care we provided is of the highest standards. We gradually grew our skilled census from an average of less than seven residents to an average of 60 skilled residents.
Three years ago, we opened a state-of-the-art rehab unit known as The Lodge at Willow Bend, which has private rooms, private baths, and an atmosphere that encourages residents to relax and enjoy their rehab stay. Voted the best rehab in Mesquite two years in a row, we are the preferred provider for numerous physicians, churches, case managers and insurance companies. From day one, our administrator and Linda always had the vision that we would be the best in Mesquite. Our leadership team is one-of-a-kind, and we all work together as a family unit. We have all stood by each other through the ups and downs, showing what it takes to build a successful team.
Anna Boone, Director of Therapy Programs: Anna brings 22 years of experience to the Willow Bend family. Anna is a member of the Ensign Leadership Council. As a member of this elite group, she is able to help pave the path along which Ensign Therapy is moving. She is also the chairperson for the Ensign CEU committee, which focuses on the education of our therapists.
Anna leads our Rehab team to excellence in clinical, customer service and financial outcomes. Willow Bend consistently rates in the top 3 percent on the weekly trend report. Our Rehab department is unsurpassed in delivering quality patient care. Being a therapist at Willow Bend means a commitment to excellence and a devotion to continuing education, which allows us to provide the highest level of innovation to our treatment approaches.
Through our continuum-of-care approach, our therapy department follows patients from their discharge from the hospital, through their skilled stay, continuing to home health and finally outpatient services. Our unique pet therapy program puts a smile on everyone’s face. Our goal as a rehab department is to keep our residents as independent as possible for as long as possible. We own it, believe it and live it. We are blessed to have the opportunity to make a difference in people’s lives every day.
Diane Shilt, Case Manager: Willow Bend was able to create a new Case Manager position distinctly designed to grow our HMO census. Diane has been able to work with our Director of Marketing and Admissions team to grow and build relationships with Case Managers at the insurance carrier level as well as the hospital referral level. Diane has extended the networking system to increase referrals by educating and reminding fellow case managers about the unique skilled services that Willow Bend can offer.
Diane has impacted the reputation that Willow Bend has with most of the major HMO insurance carriers to be positive and support their needs. Humana has designated Willow Bend as being a Star Provider of SNF services. Before Diane was the Nurse Case Manager at Willow Bend, the average HMO census was 20 beds, and since then, the HMO census has averaged as much as 36 beds in the first year that this position was created.
Most recently, Diane has taken on the Case Manager role for all of our VA contract residents. She has ensured that Willow Bend has kept within the VA guidelines and helped obtain long-term contracts to obtain continued census. Diane has been able to impact the appeals process on a local level by researching denials on HMO carriers that need to have medical necessity in order to pay correctly. Diane has impacted the outcome studies with HMO reporting for Willow Bend and promoted the managed care guidelines of service for our facility that are necessary to ensure that we are competitive as healthcare providers in today’s market.
Yolanda Reason, MDS Coordinator: Yolanda has been able to work persistently with Willow Bend’s two other MDS nurses, Ashley Jackson and Nicole Campbell, to ensure that we capture the services rendered to our residents. Their exceptional leadership is thorough, educating our floor staff on proper documentation.
Ongoing education is necessary in efforts to capture our services provided. Yolanda recently completed a staff in-service to educate and reinforce accuracy when documenting ADL care. During our daily standup meeting, the IDT receives daily reminders about the importance of timely completion of their section(s) of the MDS. Accuracy of the MDS process is evident in our routine compliance visits. Our MDS team has worked diligently to manage as many as 62 skilled residents and 147 residents overall. Our MDS team continues to play a vital role in the financial success of Willow Bend.
Mindy Rhodes, Business Office Manager: Mindy has been Willow Bend’s Business Office Manager since March 2013. She has worked diligently with her fellow business office team members, Sheryl Porter and Rebekah Martin, to completely turn our business office around at Willow Bend for the better.
We have the highest volume of HMOs in Texas. Often, more than half of all Texas Keystone HMOs are in Willow Bend at any given time. It takes longer to collect money from HMOs than it does from other payers, such as Medicare or Medicaid. We have put systems in place to stay on top of our HMO companies to ensure follow-up happens in a timely manner so that payments can be made promptly to Willow Bend. In 2013, our percentage collected was 97 percent, and in 2014, our percentage collected was 98 percent. As a team, we have dropped our bad debt percentage from 1.89 percent in 2013 to 1.51 percent in 2014. We also had an average DSO in 2013 of 47.84. In 2014, we were able to drop this percentage to an average of 42.65; this number, when adjusted for the percentage of HMOs, represents one of the best in Keystone in the Dallas area. We strive to help our family members and residents understand everything regarding the financial portion of their stay and make the financial process as easy as possible.
Sharon Wheeler, Director of Admissions: Sharon has been with Willow Bend since March 2012. We were able to see her great potential the moment she walked through our doors, and she has gradually moved from Customer Relations Specialist and Accounts Payable to one of our most successful directors of admissions.
Willow Bend has utilized Sharon’s background and marketing and her love for organization to make our admissions process as smooth and comfortable as possible for residents, family members and employees. Sharon ensures that our up to 75 admissions a month are able to call Willow Bend their home away from home, as pain-free as possible. Sharon is aware that entering a skilled nursing facility can be scary and unnerving for many residents and families. Her excellent communication skills have helped make sure that our residents are comfortable from admit to discharge. That’s saying a lot, as we had over 750 admissions in 2014.
Waylon Howard, Director of Operations: Willow Bend is blessed to have a unique Director of Operations. Waylon began as our Director of Maintenance in 2012. Since then, he has met the facility need in several areas of administration. Waylon has morphed his Director of Maintenance position into our exceptional Director of Operations.
In addition to his Maintenance Department and Life Safety/Building Safety training duties, Waylon ensures that we are in compliance with all of our Ensign U trainings, and he facilitates our Daily PPS meetings, Weekly Skilled Medicare and Part B meetings, and Triple Check meetings. Waylon is called on daily to be our Mr. Fix-It and operates as the information source for all operation needs. Waylon is a true team player and willing to do whatever is needed for Willow Bend to be successful day in and day out.
Kevin Niccum, Executive Director: Willow Bend has been privileged to have Kevin Niccum as our Administrator since 2008. Not only has he helped our facility improve financially, but he also has instilled the idea of teamwork into our department heads and leads by example for all employees.
In 2014, Willow Bend department heads finished reading as a team The Five Dysfunctions of a Team. CAPLICO has been taught many times to our leadership team and staff, and we are excited to begin studying leadership principles. Kevin has helped ensure that Willow Bend has improved year after year in almost every significant measurement. Without Kevin’s excellent leadership, the clinical and financial outcomes could not have been achieved in 2014.
Other details of note at Willow Bend include the following:
- We were at over 100 percent of our BHAG Goal at the end of December 2014.
- Our facility completed our most recent Annual State survey on Jan. 9, 2015, with some of our best results yet. We have an expectation of two low-level tags.
- We love our residents. It shows by the fact that almost all of our bread is baked fresh daily by our kitchen staff, and our vegetables are fresh, not canned or frozen.
- We love our employees, too! Promoting culture is a way of life at Willow Bend. We hear “Benders Unite” from Kevin frequently, reminding us that we are all part of one big family working together toward the same outcomes.
- One of the ways in which Willow Bend has addressed culture is in rewarding the staff who goes above and beyond their duties when it comes to resident or staff needs. We use a system called the WOW program to recognize our staff’s unrelenting hard work and dedication. WOW stands for Witnessed Outstanding Work, and we have cards readily available around the building so that staff, residents and families can help acknowledge the visible hard work in our building. When a staff member receives a WOW card, he or she is then invited to an employee recognition lunch where the cards are read, and the employees are thanked and congratulated and presented with a WOW card to be placed with their name badge so that everyone in the facility knows they were recognized.
- We have expressed culture through staff and resident talent shows, using staff to assist in the decorating of common areas to create a feeling that is more like home for both the staff and residents. During our monthly all-staff meeting, we present culture in the form of in-service or games, such as the one you will find attached. Correct answers are rewarded immediately to the answering team in the form of a gift or candy to generate excitement.
- We have a wall full of Moments of Truth, and we have an annual more prestigious award called the Pineapple Award that recognizes those who constantly show moments of truth in their everyday actions.
Here are some things we have done to promote our culture:
- We have created neighborhoods and communities within our facility where our residents live in “households” rather than living in certain “wings” or “floors,” organized around a nurse’s station. No one is called a “patient”; rather, they are called residents.
- Residents can wake up and go to sleep on their own schedule.
- You’ll see our staff knock on doors before entering a resident’s room.
- Residents have decorated their own rooms with selected belongings from home.
- You’ll find therapy dogs coming through the home for our residents to pet, birds chirping in clean cages, aquariums in the lobby and plants placed throughout the facility.
- Our residents order from menus.
- We have gathering places scattered throughout the facility so residents can read, visit with each other, watch television, play games or just sit and enjoy the ambience.
- We believe that relationships among our staff, residents and families must be continually nurtured and are vital to quality care.
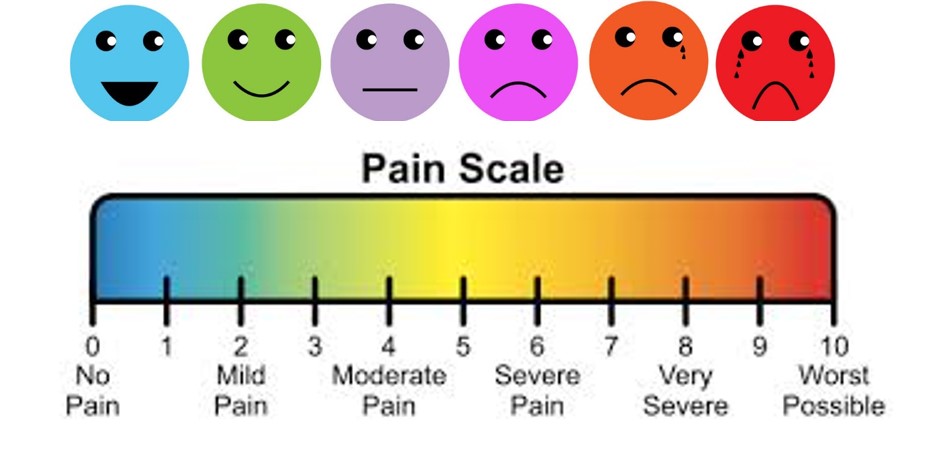
 Annual limitations on per beneficiary incurred expenses for outpatient therapy services under Medicare Part B are commonly referred to as “therapy caps.” All beneficiaries began a new cap year on January 1, 2015, since the therapy caps are determined on a calendar year basis. For physical therapy (PT) and speech-language pathology services (SLP) combined, the limit on incurred expenses is $1,940 in 2015. For occupational therapy (OT) services, the limit is $1,940 in 2015. Deductible and coinsurance amounts paid by the beneficiary for therapy services count toward the amount applied to the limit.
Annual limitations on per beneficiary incurred expenses for outpatient therapy services under Medicare Part B are commonly referred to as “therapy caps.” All beneficiaries began a new cap year on January 1, 2015, since the therapy caps are determined on a calendar year basis. For physical therapy (PT) and speech-language pathology services (SLP) combined, the limit on incurred expenses is $1,940 in 2015. For occupational therapy (OT) services, the limit is $1,940 in 2015. Deductible and coinsurance amounts paid by the beneficiary for therapy services count toward the amount applied to the limit.








 ingful activities to engage the resident and redirect their behaviors?
ingful activities to engage the resident and redirect their behaviors?