 As we move closer to the October 1st changes with PDPM, many therapy programs have made concerted efforts to implement Group and Concurrent modes of treatment and have noted how their patients are enjoying them. Since January of 2019 we can see a significant shift to adding multi-patient treatment programming across several affiliated companies. The chart below shows a steady increase month-over-month for 2019.
As we move closer to the October 1st changes with PDPM, many therapy programs have made concerted efforts to implement Group and Concurrent modes of treatment and have noted how their patients are enjoying them. Since January of 2019 we can see a significant shift to adding multi-patient treatment programming across several affiliated companies. The chart below shows a steady increase month-over-month for 2019.

So the real question is: What is the impact of group treatment to our organizations? Let’s briefly look at how these modes of treatment have an effect on Financial, Clinical and Cultural outcomes.
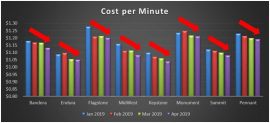
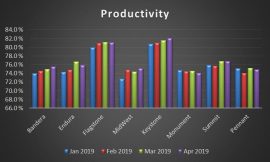
Financial:
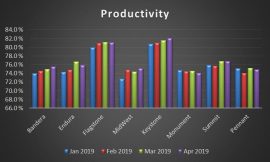
Below is an example of CPM and Productivity several markets. As you can see, being focused on providing multi-participant therapy programs created a LOWER Cost per Minute with a HIGHER Productivity (working smarter…not harder)!
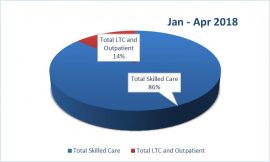
 Also, by providing multi-patient clinically appropriate treatment approaches, we create additional time to ensure we are providing care to our LTC residents and grow our outpatient programs. Note the trend from the first 4 months of 2018, to the first 4 months of 2019, as we increased our “Moments of Love” (Ciara Cox) for those that reside within our facilities and our communities from 14% to 19%!
Also, by providing multi-patient clinically appropriate treatment approaches, we create additional time to ensure we are providing care to our LTC residents and grow our outpatient programs. Note the trend from the first 4 months of 2018, to the first 4 months of 2019, as we increased our “Moments of Love” (Ciara Cox) for those that reside within our facilities and our communities from 14% to 19%!
Clinical:
Within Optima we assess each patient’s Initial and Discharge Functional status through our CARE Items sets (Physical and Occupational Therapy). Another trend we can see is a general increase in the Mobility and Self Care improvement for all patients. This is a snap-shot and requires additional study; however it is interesting to see our clinical outcomes improving as our modes of treatment are changing…
 Another area that would be great to study is the impact of Long Term Care therapy programming compared to changes in facility Quality metrics. Some markets already have been working on this and we would love to see your results!
Another area that would be great to study is the impact of Long Term Care therapy programming compared to changes in facility Quality metrics. Some markets already have been working on this and we would love to see your results!
Cultural:
How does one measure culture? Very tough question, however I believe we can look at some anecdotal evidence from the massive number of emails we all have been sharing demonstrating the creativity, functionality and joy from our therapy professionals, residents and patients. Dozens and dozens of emails from Directors of Rehab and Therapy Program Managers have been shared across all companies AND dozens more have been shared just within each market.
For those still looking for ideas about groups or evidence for the effectiveness and benefits of group programming, below is a Link to our Portal for Therapy Group list of published articles.
Portal:
Group Therapy Programming
Modes of TherapyPOSTette1
Please continue to share your ideas, reach out for support and focus on ensuring each patient and resident receives the BEST care. Thanks for all you do!
By Chad Long, Therapy Resource
Sources for the Effectiveness of Group Treatment:
Flora M. Hammond,,2 Ryan Barrett, MS, Marcel P. Dijkers, PhD, FACRM,4 Jeanne M. Zanca, PhD, MPT,5 Susan D. Horn, PhD,3 Randall J. Smout, MS,3 Tami Guerrier, CTRS,1 Elizabeth Hauser, OT,1 and Megan R. Dunning, PT, DPT, NCS6Group therapy use and its impact on the outcomes of inpatient rehabilitation following traumatic brain injury: Data from TBI-PBE project ArchMed Rehabil 2015 Aug; 96(80):S28 Phys-S292.e.5
De Weerdt W, Nuyens G, Feys H, Vansgronsveld P, VandeWinckel A, Nieuwboer A, Osaer J, Kiekens C. Group physiotherapy improves time use by patients with stroke in rehabilitation. Aust J Physiother. 2001;47:53–61. [PubMed]
Kurasik S. Group dynamics in the rehabilitation of hemiplegic patients. J Am Geriatr Soc. 1967;15:852–5. [PubMed]
Trahey PJ. A comparison of the cost-effectiveness of 2 types of occupational-therapy services. Am J Occup Ther. 1991;45:397–400. [PubMed]
Coulter CL, Weber JM, Scarvell JM. Group physiotherapy provides similar outcomes for participants after joint replacement surgery as 1-to-1 physiotherapy: a sequential cohort study. Arch Phys Med Rehabil. 2009;90:1727–33. [PubMed]
Zanca JM, Dijkers MP, Hsieh CH, Heinemann AW, Horn SD, Smout RJ, Backus D. Group therapy utilization in inpatient spinal cord injury rehabilitation. Arch Phys Med Rehabil. 2013;94:S145–S153. [PubMed]
Oouchida Y, Suzuki E, Aizu A, Takeuchi N, Izumi S. Applications of Observational Learning in Neurorehabilitation. Int J Phys Med Rehabil. 2013;1(5):1–6.
Gauthier L, Dalziel S, Gauthier S. The benefits of group occupational therapy for patients with Parkinson’s disease. Am J Occup Ther. 1987;41:360–5. [PubMed]
Dobrez DG, Lo Sasso AT, Heinemann AW. The effect of prospective payment on rehabilitative care. Arch Phys Med Rehabil. 2004;85:1909–1914. [PubMed]
Fuller PR. Matching clients to group therapies. J Psychosocial Nursing. 2013;51:22–27. [PubMed]
 Did you know….
Did you know….






 Deciding the Principle Medical Diagnosis, By Lori O’Hara, MA, CCC-SLP
Deciding the Principle Medical Diagnosis, By Lori O’Hara, MA, CCC-SLP
 As we move closer to the October 1st changes with PDPM, many therapy programs have made concerted efforts to implement Group and Concurrent modes of treatment and have noted how their patients are enjoying them. Since January of 2019 we can see a significant shift to adding multi-patient treatment programming across several affiliated companies. The chart below shows a steady increase month-over-month for 2019.
As we move closer to the October 1st changes with PDPM, many therapy programs have made concerted efforts to implement Group and Concurrent modes of treatment and have noted how their patients are enjoying them. Since January of 2019 we can see a significant shift to adding multi-patient treatment programming across several affiliated companies. The chart below shows a steady increase month-over-month for 2019.
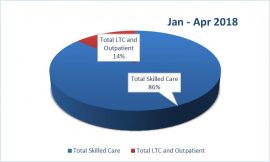
 Also, by providing multi-patient clinically appropriate treatment approaches, we create additional time to ensure we are providing care to our LTC residents and grow our outpatient programs. Note the trend from the first 4 months of 2018, to the first 4 months of 2019, as we increased our “Moments of Love” (Ciara Cox) for those that reside within our facilities and our communities from 14% to 19%!
Also, by providing multi-patient clinically appropriate treatment approaches, we create additional time to ensure we are providing care to our LTC residents and grow our outpatient programs. Note the trend from the first 4 months of 2018, to the first 4 months of 2019, as we increased our “Moments of Love” (Ciara Cox) for those that reside within our facilities and our communities from 14% to 19%!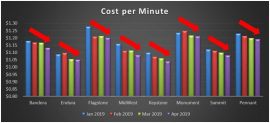
 Another area that would be great to study is the impact of Long Term Care therapy programming compared to changes in facility Quality metrics. Some markets already have been working on this and we would love to see your results!
Another area that would be great to study is the impact of Long Term Care therapy programming compared to changes in facility Quality metrics. Some markets already have been working on this and we would love to see your results! Pointe Meadows of Lehi, Utah uses the game, Headbands, in an SLP group. Headbands can be used to facilitate turn taking, processing speed, expressive communication, reading comprehension, and speech intelligibility
Pointe Meadows of Lehi, Utah uses the game, Headbands, in an SLP group. Headbands can be used to facilitate turn taking, processing speed, expressive communication, reading comprehension, and speech intelligibility