Submitted by Jennifer Raymond, Therapy Resource — Northern CA
 In January, Elyse Matson, MA CCC-SLP, Speech Language Pathology Resource/Ensign Services, provided an onsite half-day training course for the Flagstone NorCal Market Speech Language Pathologists and DORs.
In January, Elyse Matson, MA CCC-SLP, Speech Language Pathology Resource/Ensign Services, provided an onsite half-day training course for the Flagstone NorCal Market Speech Language Pathologists and DORs.
The training content focused on how PDPM has changed SLP practice, including review of PDPM and SLP case mix, use of group and concurrent therapy, clinical documentation for both skilled and LTC patients, coding/goal writing, standardized testing, Medicare Part B utilization, dementia treatment utilizing Abilities Care, and the latest evidence-based practice and treatment techniques.
Since all of the SLPs in the NorCal market work independently in their facilities and many of them are geographically far apart, these therapists rarely are able to collaborate with each other in person. The course was an opportunity for them to meet face-to-face (some for the first time), share a meal, ask questions and discuss best practices with their colleagues, and update their learning together.
The course was enthusiastically received by our SLPs, as demonstrated in their comments below:
- “I feel more confident in documenting skilled services, great use of resources”
- “I have more tools now for providing abilities-based care”
- “I have learned new coding and documentation skills”
- “I feel more comfortable treating patients with dementia”
- “Now I really understand the increased role of SLP with PDPM”
- “Going forward, I know how to make my goals more specific on my POC”
- “Wonderful learning and networking afternoon; can we please do this at least every six months?”
In addition, by inviting the non-SLP DORs, it provided an opportunity for our OT and PT leaders to have a better understanding of the broad range of available ST clinical services, documentation requirements and processes specific to PDPM and LTC interventions for their SLP programs.
JB Chua, PT/DOR for Summerfield, shared:
“Attending the SLP training course gave me tools on how to support my SLP in growing our program. It gave me insight on what to look for during our Daily Technical Meeting. Triggers that will make me ask my SLP to screen a particular patient to help us capture an accurate clinical picture of our patients. Lastly, it also helped me understand words/phrases that SLPs use that a PT seldom or never uses in their documentation. Overall, this training course is highly recommended not only for our awesome SLPs, but most especially for DORs without an SLP background.”
Thank you, Elyse, for this opportunity to exercise our Passion for Learning in NorCal!




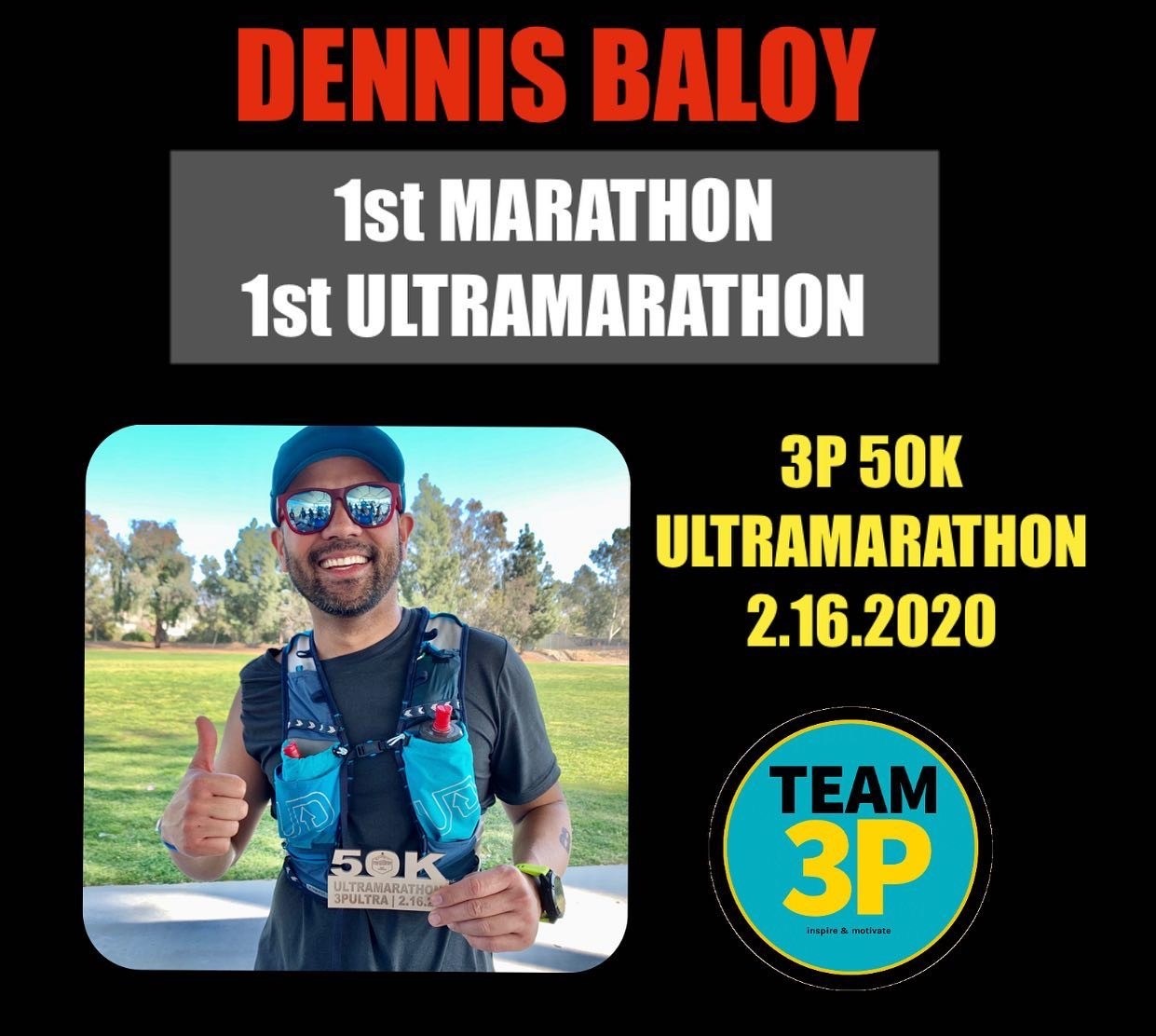
 Discovering running at a much later stage in life has been the greatest gift life has given me. It came at a perfect time when I needed a lift, to be reminded of my life’s purpose and overcome my self-imposed limitations. Running has given me everything … my renewed self-love, my self-confidence, my fearlessness, my grateful attitude and my purpose. It has inspired my new direction and outlook. It has taught me to push forward when things get difficult. In return, I am giving it my heart.
Discovering running at a much later stage in life has been the greatest gift life has given me. It came at a perfect time when I needed a lift, to be reminded of my life’s purpose and overcome my self-imposed limitations. Running has given me everything … my renewed self-love, my self-confidence, my fearlessness, my grateful attitude and my purpose. It has inspired my new direction and outlook. It has taught me to push forward when things get difficult. In return, I am giving it my heart. In March 2017, I ran my first individual race, which was a half marathon with my sister. We decided to follow the 2:30 pacer. I wasn’t serious about it at first, conversing with her while running, answering texts during the race until around mile 8-9 when I saw how serious and competitive other runners were and thought to myself that maybe I should take it more seriously, too. I started giving it my best and got ahead of the 2:15 pacer to the finish. This race gave me a glimpse of the possibilities, although a full marathon was still out of the picture at that time.
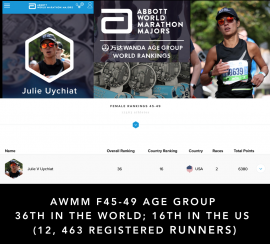
In March 2017, I ran my first individual race, which was a half marathon with my sister. We decided to follow the 2:30 pacer. I wasn’t serious about it at first, conversing with her while running, answering texts during the race until around mile 8-9 when I saw how serious and competitive other runners were and thought to myself that maybe I should take it more seriously, too. I started giving it my best and got ahead of the 2:15 pacer to the finish. This race gave me a glimpse of the possibilities, although a full marathon was still out of the picture at that time. currently chasing the 6 Major Marathons in the world and since 2018 have completed four of six (Berlin, Chicago, Boston and New York). From these races, I have earned a respectable world ranking and received an invite to run the Wanda Age Group World Championships inaugural race in London this April. This is where I will be competing against 84 other top world runners in my age group.
currently chasing the 6 Major Marathons in the world and since 2018 have completed four of six (Berlin, Chicago, Boston and New York). From these races, I have earned a respectable world ranking and received an invite to run the Wanda Age Group World Championships inaugural race in London this April. This is where I will be competing against 84 other top world runners in my age group.